Gum health is often the unsung hero of oral care, frequently underestimated by patients and, at times, under-prioritised in general practice. Yet, as our understanding of periodontal disease evolves, one thing is clear: healthy gums are not only the bedrock of a functional, aesthetic smile, but a critical component of overall systemic health.
For general dentists, this shift in understanding presents both a professional responsibility and a strategic opportunity. Early detection and effective management of periodontal disease can drastically improve patient outcomes, reducing the risk of tooth loss, systemic complications, and long-term treatment burdens. From a practice perspective, prioritising gum health supports a culture of preventive care, drives long-term patient retention, and contributes to a more robust model of dentistry.
At the forefront of this movement is Dr Reena Wadia, a leading figure in periodontology and one of the UK’s most respected voices on gum health. A former associate specialist at Guy’s Hospital and now Founder & CEO of RW Perio, an award-winning specialist referral clinic in London, Reena has long championed the idea that gum care is not a niche concern, but a central pillar of modern dentistry. Through the Perio School, she also trains and mentors dentists and hygienists from around the world, empowering them to integrate high-quality periodontal care into everyday practice.
Dr Reena’s approach is clear, collaborative, and deeply rooted in patient-centric care. She believes that empowering patients with knowledge, translating clinical concepts into everyday language, and embedding consistent preventive strategies across the dental team can radically improve engagement and outcomes. For Reena, gum health is more than a treatment category; it’s a mindset that needs to be woven into every aspect of practice, from the reception desk to the dental chair.

In this exclusive Q&A, Dr Reena shares her thoughts on how dental teams can communicate the value of periodontal care, align with the latest research on systemic health, and implement practical, scalable changes to elevate gum health within general dentistry. She also offers her insights on the future of periodontics, and why now, more than ever, this area of care deserves our full attention.
Gum health is often overlooked by patients - how can dental practices shift the conversation to help patients see it as a key part of their overall well-being?
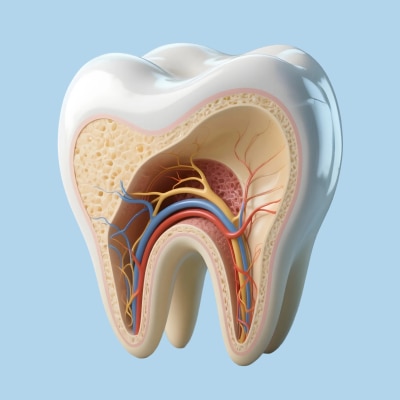
Dr Reena Wadia: It starts with communication and language. I’ve always found translating key messages super helpful. For example, instead of talking about “just a scale and polish,” we need to explain what’s really happening - highlighting the inflammation, the biofilm, and how it all connects to the rest of the body.
Patients don’t want plaque removed - they want to stay healthy, feel confident, and prevent long-term problems. The key is consistent messaging from the whole team, visuals to show progress, and reframing gum care as something proactive and empowering.
We know that periodontal health is linked to systemic conditions like heart disease and diabetes - how can dental professionals better communicate these links to encourage preventive care?
RW: It’s about bringing science into the everyday conversation. Patients are often surprised when we mention the connection between bleeding gums and systemic inflammation. We can use analogies - for example, explaining that the mouth is a mirror to the rest of the body, and gum inflammation is like a silent alarm.
A simple line like “your gums could be telling us something about your overall health” can be incredibly powerful. And screening for things like diabetes through gum health is a game-changer.

RW Perio has built an incredible reputation as a leading gum health clinic. What are some practical strategies that general dental practices can implement to improve outcomes for their perio patients?
RW: First, early diagnosis. Always record the BPE and use the updated classification system. Second, structured systems - whether that’s recalls, supportive care, or documentation, consistency matters. And third, elevate your hygiene team. Invest in their development, ensure they feel empowered, and create seamless communication between them and the dentist.
A strong team culture makes a huge difference in periodontal outcomes.
Preventive dentistry is key to reducing periodontal disease - what do you see as the most effective ways for dental teams to integrate better prevention strategies into daily practice?
RW: It’s all about embedding prevention into every patient touchpoint - from reception to the chair. Simple tweaks like motivational interviewing, using before-and-after photos, or giving personalised home care advice that patients actually understand and remember, go a long way.
Also, tracking progress - whether through plaque and bleeding scores or photos helps patients stay accountable and engaged.
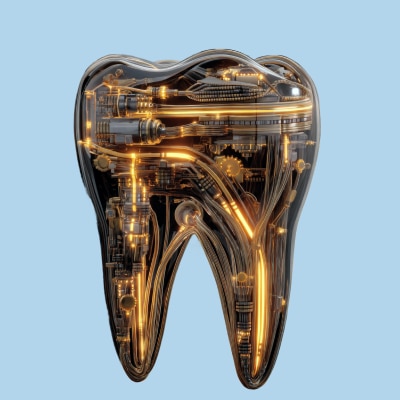
Looking ahead, what exciting advancements or shifts in periodontics do you think will have the biggest impact on the future of dentistry?
RW: We’re seeing a huge move toward personalised care especially when it comes to risk profile. There’s also a greater focus on non-invasive tech that enhances biofilm disruption and better diagnostics that give us earlier insights.
I also think perio is finally getting the attention it deserves - with systemic health links making it more relevant than ever.